Zenocutuzumab is a novel bispecific antibody designed by Merus, N.V. In a multicenter global phase 2 clinical trial led by MSK gynecologic medical oncologist and early drug development specialist Alison Schram, MD, the drug demonstrated durable antitumor activity and met prespecified goals for outstanding activity.
Dr. Schram and co-investigators have now published findings from the eNRGy study, the phase 2 component of the open-label phase 1/2 study of zenocutuzumab in adult patients with advanced or metastatic NRG1+ solid tumors (NCT02912949), in The New England Journal of Medicine. (1)
Responses to zenocutuzumab were observed in several tumor types, with notable responses in patients with NSCLC (29%) and pancreatic adenocarcinoma (42%). Treatment-related adverse events were mainly low-grade. (1)
“These results are particularly exciting because NRG1+ lung cancers typically do not respond to standard chemotherapy or immunotherapy and there are no approved targeted treatments for this patient population,” said Dr. Schram. “While treatment with zenocutuzumab is not curative, durable antitumor activity and low toxicity are clinically meaningful benefits, especially for patients with cancer that has progressed on standard treatments.”
MSK was heavily involved in preclinical and translational research into NRG1 fusions, the formation of the global eNRGy1 patient registry, and the development of the clinical trial design. Merus N.V. is sponsoring the ongoing study, which continues to recruit patients worldwide.
NRG1 Fusions
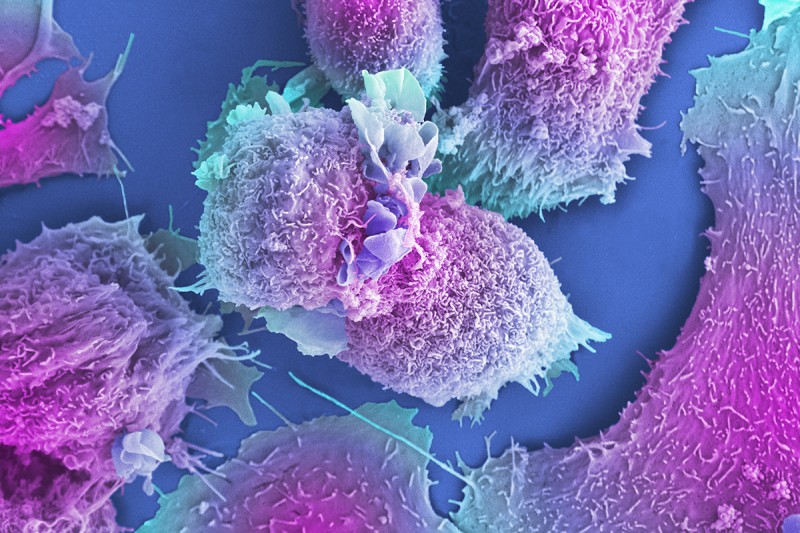
NRG1 rearrangements are rare, occurring in less than 1% of solid tumors. However, they have been identified in diverse cancers, (2) (3) and are found more frequently in invasive mucinous adenocarcinoma of the lung and KRAS-wild type pancreatic adenocarcinoma. (4-11) NRG1 fusion proteins bind to human epidermal growth factor receptor 3 (HER3), triggering HER2-HER3 heterodimerization and activating downstream cancer growth and proliferation. (9) (12)
Zenocutuzumab and How it Works
Zenocutuzumab is a first-in-class, humanized, full-length immunoglobulin G1 bispecific antibody that targets HER2 and HER3 directly. After docking on HER2, the drug blocks HER2-HER3 dimerization and NRG1 fusion proteins from interacting with HER3, suppressing tumor cell growth and survival. (1) The drug also plays a role in antibody-dependent cellular cytoxicity. (13) It is delivered in an intravenous infusion every two weeks until disease progression.
MSK’s Pioneering Work in NRG1 Fusion-Positive Cancers
“MSK has been a leader in describing NRG1 fusion biology, identifying strategies to target this alteration, and concept development for clinical trials in this patient population,” said Dr. Schram.
MSK’s research into NRG1+ cancer began many years ago with a single patient treated on a different clinical trial. The patient’s tumor responded to a HER3 monoclonal antibody, as described in a 2018 case report by MSK thoracic medical oncologist and early drug development specialist Alexander Drilon, MD and colleagues. (9) Dr. Drilon also led the development of the global eNRGy1 registry, a consortium of 22 centers from nine countries in Europe, Asia, and the United States contributing data from patients with NRG1+ lung cancers. (12) The Mark Ladanyi Lab investigated the biological processes of NRG1 fusions and how to target them.
At the same time, Merus was developing zenocutuzumab for patients with HER2 overexpression. Dr. Schram and Merus began collaborating on the development of zenocutuzumab in the NRG1+ patient population in 2019.
Study Design
Eligible patients had received standard therapy or were not considered candidates for standard therapy and had NRG1+ fusions identified by next-generation sequencing through local testing at Clinical Laboratory Improvement Amendments (CLIA)-certified laboratory or equivalent. (1)
A total of 39 distinct NRG1 fusion partners were identified across study participants — mainly by RNA-based next-generation sequencing (86% of patients). Interestingly, 40 of 42 treated patients (95%) with NRG1+ pancreatic cancer had KRAS wild-type disease. (1)
“Most DNA panels do not include NRG1 because its introns are very large. MSK-IMPACT®, for example, will detect some cases, but only when an upstream partner, such as CD74, is captured on the panel. By contrast, RNA sequencing can identify NRG1 explicitly,” said Dr. Schram, who was also the lead author of the paper. “The take-home message is that if a patient has a driver-negative lung or pancreatic tumor on DNA sequencing, it’s important to perform RNA sequencing.”
Tumor assessments by computed tomography or magnetic resonance imaging were conducted at baseline and every eight weeks until disease progression. The primary end point was overall response rate (ORR). The main secondary end point was duration of response. Other secondary end points included time to response, progression-free survival (PFS), safety, pharmacokinetics, and immunogenicity. (1)
Study Results
The median age of patients enrolled in the study was 62 years and 60% of patients were female. Most patients (82 of 94, or 87%) had received prior systemic therapy, including platinum-based chemotherapy, immunotherapy, and afatinib, and 72 patients or 77% had received treatment for metastatic disease. Almost all patients with pancreatic cancer who were evaluable for efficacy, 35 of 36, had received prior systemic therapy (FOLFORINOX and/or gemcitabine/taxane) and 33 had received systemic therapy for metastatic disease. (1)
Overall, among 158 patients with measurable NRG1+ cancer in various tumor types who were enrolled at least six months before the data cutoff date, 47 had a response, producing an ORR of 30%, with a median duration of response of 11.1 months and 19% of responses ongoing. The median time to response was 1.8 months, and the median PFS was 6.8 months. (1)
For patients with NRG1+ NSCLC, the response rate was 29% (27 of 94 patients), with a median duration of response of 12.7 months. For patients with NRG1+ pancreatic cancer who were evaluable for efficacy, the response rate was 42% (15 of 36 patients). The median duration of response was 7.4 months and the median PFS was 9.2 months. (1)
The most common treatment-related adverse events were diarrhea (18% of patients), fatigue (12%), and nausea (11%). One patient discontinued treatment due to grade 2 pneumonitis associated with treatment. (1)
MSK Research Continues
Dr. Schram and co-investigators at MSK are now looking at mechanisms of resistance and alternative methods for targeting NRG1+ fusions. She noted that she is also working on efforts describing the demographics, genomics, and the natural history of NRG1 fusion-positivity in patients treated at MSK.
The study was funded by Merus, N.V. Dr. Schram’s translational research was supported by a Career Development Award from the American Society of Clinical Oncology an Cycle for Survival® grant. Access disclosures for Dr. Schram.